Lean Mass Hyper Responders And Heart Disease Risk
Jan 27, 2025
Are Lean Mass Hyper Responders At Higher Risk For Heart Disease?
There is this movement online where people who eat very low carb, eat mostly meat and fat, including saturated fat, think that they cannot get heart disease because they are “metabolically healthy”. They define this as having high HDL, low triglycerides, and often extremely elevated LDL-C. They call this phenotype “Lean Mass Hyper Responders”.
It’s important to note that in their own studies, they state that you don’t actually have to be lean. It’s unclear then why this is called “lean” mass. They also have not done dexa scans nor MRIs to determine leanness.
Lean Mass Hyper Responders And Cholesterol
Nearly every study that has looked at LDL-C, including many that I have discussed in this book, included these young, healthy people, who have elevated LDL-C due to eating a lipid elevating diet.
What if we took out that subset of the population and looked at them specifically?
Dr. Deirdre Tobias is an Assistant Professor in the Department of Nutrition at Harvard University. She is an obesity and nutrition epidemiologist. She set out to answer this exact question. As a specialist in epidemiology, she is an expert in this field and in data analysis. Yes, it’s been answered before. But she wanted to be absolutely certain and provide a detailed review of this topic.
Dr. Tobias bio:
https://www.hsph.harvard.edu/profile/deirdre-kay-tobias/

She conducted this analysis on the Women’s Health Study database. They excluded women with prior CVD, cancer, or diabetes. She wanted only “metabolically healthy” participants. She ended up with 19,057 women in her cohort for analysis. These were women with normal blood sugars, low triglycerides, high HDL-C, and an LDL-C level available for analysis.
The “metabolically healthy” women she analyzed were (from her paper):
• Leaner
• More educated
• Higher income
• Not a current smoker
• Active
• Drinkers
As the LDL-C went higher and higher, the women were older, higher BMI, postmenopausal, and had modestly lower education and income. She adjusted for these confounders.
She evaluated baseline lipids, follow up lipids, and long term follow up (20+ years) for death. She obviously removed statin users.
The overall population was stratified based on their HDL-C and triglycerides. They had to have HDL-C equal or greater than 50 mg/dL and TG < 100 mg/dL. She then divided the participants based on highest and lowest LDL-C quintiles. Quintiles means dividing a cohort into 5 groups, the top 20%, the next 20%, and so on until you have 5 cohorts each comprising the next lowest or highest 20%.
She adjusted for smoking, obesity, BMI, age, and other confounders.

This was the result. The pink line at the bottom is the survival curve of those with the highest LDL-C. The highest quintile had the lowest survival. You started to see separation at around the 5 year mark.
The higher the LDL-C, the lower the survival.
What if she went stricter? What about if we wanted only the very best “metabolically healthy” individuals?
She removed people with hypertension, BMI over 25, and A1c over 6.5. Here’s that survival chart. Except that the difference between the highest and lowest quintiles was even more profound.

Her conclusions were very clear, women with higher LDL-C, regardless of many other metabolic factors, were more likely to die during follow-up.
This isn’t news. We have known for years that elevated LDL-C, regardless of anything else, increases CV and all-cause mortality. The higher your LDL-C, the more likely you are to die. And sooner!
But this was one way to make it absolutely clear for the LDL-C and cholesterol disputers.
You can access her paper, charts, graphs, and research in the supplemental info that comes with this book when you go to: https://dralo.net/lipids and download the bonus material.
Lean Athletes and Cholesterol Heart Disease Risk
Another great article on this topic was done at THE Ohio State University and is titled:
The Effects of Carbohydrate versus Fat Restriction on Lipid Profiles in Highly Trained, Recreational Distance Runners: A Randomized, Cross-Over Trial
This was a trial on very lean, super athletic individuals who started out on a high carb/low fat diet and switched over to a low carb/high fat diet. They measured the lipid profiles of these athletes. This was not a huge trial by any means, they included only 7 athletes.
They concluded that healthy athletes with no prior cholesterol problems on a low carb/high fat diet demonstrated elevated LDL-C and HDL-C concentrations.

Charts A, B, and C are the charts that plotted Total Cholesterol, LDL-C, and HDL-C. You notice that all of them went up. We know what happens when LDL-C is elevated for decades, even in otherwise healthy runners. They had a 38% increase in LDL-C. Even their triglycerides went up.
Read the study:
https://pubmed.ncbi.nlm.nih.gov/35334791/
Young Lean Mass Hyper Responders Cholesterol Atherosclerosis and Heart Disease
In perhaps the most compelling study ever done on young people with no prior history of CVD, the PESA (Prevention of Early Subclinical Atherosclerosis) looked to answer this exact question. What if we examined young people with no known ASCVD and tried to assess their risk?
They looked at 4185 participants with a mean age of 45. Only 15% of them were obese, 37% were women, and they used 16 types of very fancy imaging to assess ASCVD in 5 different vascular beds. These imaging techniques are not available to most clinicians and are used in research labs. They are quite expensive. Only 18% had a calcium artery score that was positive (0-99).

Even more interestingly, they found that 45% of people with a “normal” LDL-C of 110 mg/dL had ASCVD. When the LDL-C was at the upper limit of “normal” at 130 mg/dL, 58% had ASCVD. When you looked at LDL-C of 150 mg/dL, 64% of participants had ASCVD. The current recommended upper limit of normal is no longer 130 mg/dL, it has been lowered to 100 mg/dL, and should be even lower.

They found that 63% of all participants had ASCVD in at least one arterial bed. Of those with ASCVD in one bed, approximately 63% had ASCVD in more than one arterial bed.
They also found that of those with a CAC score of 0, 60% had subclinical ASCVD in at least one arterial bed.
Further, the Framingham 10-Year Risk Score of most participants was 6% and most participants (85%) were considered “low risk” based on traditional risk calculators. That’s a lot to think about. Based on this 10-year risk score, they would not have been placed on lipid lowering therapy despite having extensive disease.
I would recommend pulling up the study or the supplemental guide to look at the images from the study.
In the PESA trial, you’ll notice that at a “normal” LDL-C of 110 mg/dL, 45% of participants had ASCVD and it goes up to 64% as you approach 150 mg/dL. This is in a population that is otherwise thought to be low risk and healthy with no obesity, no calcium, and no traditional risk factors. Even the risk calculators calculate their 10-year risk score at 6%, which is below the 7.5% or 10% that is required to recommend medications and interventions.
Also, note that people with an LDL-C below 60 mg/dL had no ASCVD. This confirms the findings of the JUPITER trial that showed that an LDL-C below about 57 mg/dL, and you can nearly eliminate ASCVD risk.

The take home message is that even in young, healthy individuals LDL-C is what matters. Regardless of how healthy you are, you have plaque in at least one arterial bed, and up to 63% of those people have it in more than one arterial bed.
Read the full results:
https://www.sciencedirect.com/science/article/pii/S0735109721051159
Healthy But Full Of Disease
In November of 2023 an update was published to the PESA trial and showed that in only 6 years, 3DIVUS was able to show significant plaque progression in these young people, who are otherwise healthy, but just had high LDL-C.
They found that if you treat high LDL cholesterol and blood pressure sooner and earlier, you can see some plaque regression in just 6 years.

In this trial, the risk factor showing the strongest association with progression of plaque was higher baseline LDL-C.
The impact of higher LDL cholesterol and higher systolic blood pressure on subclinical atherosclerosis progression was more marked in younger participants.
Regression of plaque occurred in 8.0% of individuals with prevalent disease at enrollment. The chances of 6-year regression of subclinical atherosclerosis was inversely related to baseline active smoking, male sex, higher fibrinogen, higher LDL-C, and older age.
I highly recommend looking at the graphics from this study.
Study:
https://www.jacc.org/doi/10.1016/j.jacc.2023.09.814
Health 18 Year Olds With Heart Disease: CARDIA Trial
Similarly, the CARDIA trial looked at 5115 young men (age 18-30) who were also healthy and followed them for 35 years. They examined many factors, one of which was LDL-C over time.

LDL-C exposure before the age of 40 was associated with increased ASCVD after age 40. They found a 20% reduction in CVD risk for every 1 mg/dL reduction in LDL-C of cumulative exposure. As an example, if person A has an LDL-C of 100 mg/dL for 10 years, that’s 1000 mg/dL/years of exposure. Person B has an LDL-C of 101 mg/dL for 10 years, they have 1010 mg/dL/years of exposure. That extra 1 mg/dL over 10 years increased their relative risk of ASCVD by 20% after the age 40.
They also found that the higher the exposure at a younger age accounted for worse ASCVD after age 40. The recommendation would be to treat it sooner, and lower in your 20s and 30s to avoid serious ASCVD in your 40s and beyond.
The authors concluded, “These findings indicate that both cumulative exposure and exposure that happens earlier in young adulthood are more important contributors to mid-life CVD events than later concentrations, with potential implications for early life primordial prevention strategies”.
They also found that only 10% of participants had a positive CAC by year 15 of follow-up. Meaning most participants essentially had very little “late stage ASCVD” but they must have had plenty of soft, undetectable plaque.
They also found that those with the lowest LDL-C (below 90 mg/dL) had a negative time to first visit. This means that low LDL-C conferred protection and delayed the expected onset of disease compared to their cohorts with higher LDL-C levels.
They also found that those with higher LDL-C (110-130 mg/dL) had ever increasing, earlier, and worse ASCVD compared to the rest.

Read the full study:
https://www.jacc.org/doi/10.1016/j.jacc.2021.05.022
Read the analysis of just LDL-C exposure area under the curve risk in CARDIA study:
https://www.jacc.org/doi/10.1016/j.jacc.2020.07.059
In the area under the curve (AUC) study, they stress that the longer you are exposed to high LDL-C for a longer period of time, especially in your earlier years, the worse the incident ASCVD when you are older.

The authors conclude, “Incident CVD event risk depends on cumulative prior exposure to LDL-C, measured by the area under the LDL-C versus age curve and, independently, on the time course of area accumulation. The same area accumulated at a younger age, compared with an older age, resulted in a greater risk increase, emphasizing the importance of optimal LDL-C control starting early in life”.
The higher your cumulative exposure to LDL-C from ages 18-40, the higher the chance of having incident ASCVD by age 40. Obviously, the group represented by the highest cumulative exposure to high LDL-C had the highest rates and incidence of CVD. Those with the highest LDL-C had a 3X risk of CVD than those with the lowest LDL-C.
If you need more evidence, the population in the Lyon Diet Heart Study had an average BMI of 26 kg/m2, an average A1c of 4.6%, and less than 18% of them smoked. You know what they did have? Their LDL-C averaged over 160 mg/dL. This was a secondary prevention trial. These young, lean, insulin sensitive individuals all had a heart attack. I discuss this study at length elsewhere. The only thing they had was that their LDL-C was extremely elevated.
A study from January 2024 looked at people in the UK Biobank with a genetic mutation, ANGPTL3, that keeps their triglycerides very low. They had ASCVD proportional to their apoB. ASCVD was not lower. Medications that target only triglycerides, without a reduction in apoB, have failed to reduce ASCVD risk. Hence, no guideline recommends this.
Study:
https://academic.oup.com/eurheartj/advance-article-abstract/doi/10.1093/eurheartj/ehad845/7578379
51 Year Old Lean Mass Hyper Responder Shows Rapid Progression of CAD
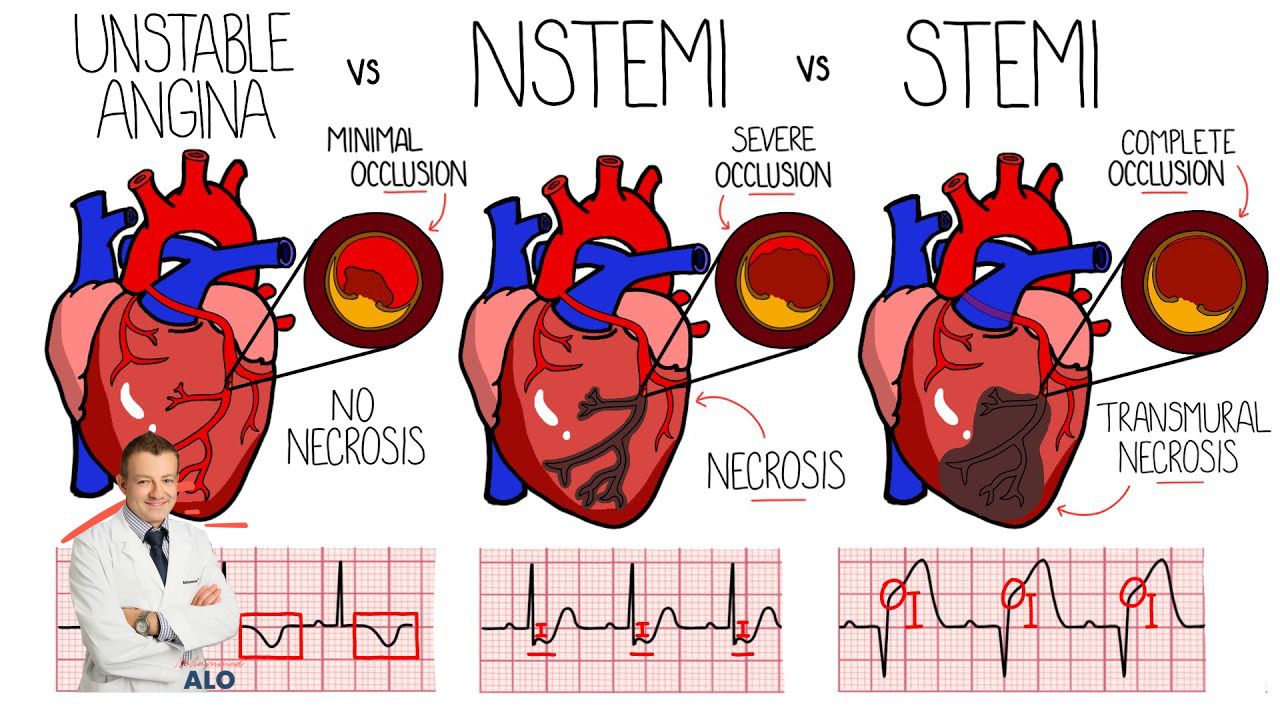
Another case report of a 51 year old male “lean mass hyper responder” showed rapid progression of his CAD after stopping statin therapy and adopting a ketogenic diet. He was quite lean with a BMI of 23. He had a history of a prior stent to his LAD two years prior. He had stopped his atorvastatin due to myalgias and adopted a ketogenic diet. His LDL-C was 301 mg/dL, HDL-C was 73 mg/dL, and TG was 71 mg/dL off statins. Two years after stopping the statin, he had a “massive” heart attack (STEMI) with a 99% blocked right coronary artery (RCA). He was treated with two stents. He was placed on Repatha (PCSK9) and sent home with an LDL-C of 14 mg/dL.
Case report:
https://www.ahajournals.org/doi/10.1161/circ.148.suppl_1.17807
A recent state of the art review from March 2024 evaluated the ketogenic diet and concluded that, “it does not meet the criteria for a healthy diet” after extensive research.

Review:
https://pubmed.ncbi.nlm.nih.gov/38232923/
For all of those claiming they are “metabolically healthy”, and that high LDL-C doesn’t matter if your HDL-C is high or your triglycerides are low, please show them this data.
Without a shadow of a doubt, high LDL-C causes ASCVD and you are at risk based on your cumulative exposure to high levels of LDL-C over the years. Especially, if it began when you were a teenager.
Another claim they make is that you cannot get heart disease without insulin resistance. They even go as far as to say that it’s not the cholesterol that causes heart disease, that it is the insulin resistance that causes heart disease. If that’s the case, why is it that only 25% of heart attack patients have insulin resistance? How about the other 75%? They don’t have insulin resistance but still had acute coronary syndrome. How do you explain that?
Study:
https://pubmed.ncbi.nlm.nih.gov/35245735/
What About Lipid and Cholesterol Markers in Lean Mass Hyper Responders?
Another study published in March of 2024 wanted to evaluate the impact of optimal cholesterol levels on subclinical atherosclerosis in young adults that do not have traditional cardiovascular risk factors.
They looked at a subgroup from the CARDIA trial age 32-46 years of age that did not have diabetes, hypertension, smoking, and dyslipidemia. Within that population, they compared two groups. One had optimal lipids and the other had suboptimal lipids.

The group with the higher LDL-C, total cholesterol, non-HDL-C had a 30-36% higher risk of CAC presence, incidence, and progression. They also had a 42-44% higher CIMT thickness. They repeated the analysis in those with a CAC score of 0 and it did not alter the results. Those with the highest LDL-C had more ASCVD regardless of CAC score.
They also found that for every 1 standard deviation of total cholesterol, LDL-C, and non-HDL-C you had a 30-36% increase in presence, incidence, and progression of CAC and a 42-44% greater odds of composite mean CIMT.
In those with a normal starting lipid panel (LDL-C < 100) at baseline, for every 1 standard deviation increase in LDL-C, you had a 108-270% increase in CAC incidence. These patients were followed for 20 years. It’s a very in depth study.
Study:
https://www.atherosclerosis-journal.com/article/S0021-9150(24)00080-7/abstract
In April of 2024, the Journal of the American College of Cardiology published a research article looking at high fat, low carbohydrate (LCHF) diets in the UK Biobank cohort. They were evaluating apoB and LDL-C in matched cohorts.

After 11.8 years of follow up, 9.8% of those on LFHC diets had a major cardiovascular event, while only 4.3% of those on a standard diet had a MACE event. After adjusting for other CV factors, the risk remained significantly and showed a 2.18X risk.
They also noted that 11.1% of those on the LCHF and only 6.2% of those on a standard diet had “severe hyperlipidemia” with LDL-C over 193 mg/dL (5 mmol/L).
In September of 2024 another analysis of the CARDIA trial looking at otherwise healthy individuals ages 18-36 found that LDL-C > 118 mg/dL and non-HDL-C < 135 mg/dL (apoB) were the best predictors of likelihood to develop ASCVD. They also stated that the earlier lipids were addressed, the less likely ASCVD to develop.
Study:
https://www.jacc.org/doi/10.1016/j.jacc.2024.06.029
Dr. Michael Mindrum recently critiqued an accepted paper on LMHR and was very critical of their manuscript because the authors did not understand lipid metabolism very well and they downplayed the causal role of LDL-C and apoB containing lipoproteins in atherosclerosis.
Critique:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9154254/
Multiple other critiques of their methodology, lack of statistical acumen, and data analysis have been published. In this critique, Javier Gonzalez discusses “invalidating errors that were made” in their meta-analysis on low carb diets, BMI, and LDL-C response to diets based on body mass subgroup analysis. If you enjoy diving deep into data and statistics, you can read the full manuscript. He also posted it on his Twitter (X) account. You cannot trust research from a group of researchers once they have had multiple papers published with data errors and redactions. Keven Hall also recently critiqued one of their publications that tried to re analyze one of his papers. They had multiple statistical errors and data falsification.
Study:
https://www.sciencedirect.com/science/article/abs/pii/S0002916524004787
Another study looked at young adults and found that non-HDL-C (apoB) cumulative exposure predicted ASCVD and events.

Time Non-HDL Measurements in Young Adults Strongly Predict Cumulative Exposure
"For adults ages 18 to 30 years, non–high-density lipoprotein cholesterol (non–HDL-C) levels above 135 mg/dL strongly predict membership in the top quartile of atherogenic lipid exposure by age 40 years. Being in this top quartile is a strong determinant of atherosclerotic cardiovascular disease (ASCVD) events after age 40 years. This study suggests that evaluating lipid-associated ASCVD risk in young adults requires considering lower absolute non–HDL-C levels than those used to define 'elevated' levels in middle-aged and older adults."
"As expected, membership in the highest quartile of 1-time measurement on non–HDL-C and LDL-C obtained between ages 18 and 30 years and the cumulative exposure from age 18 to 40 years was strongly associated with ASCVD event risk after age 40 years when compared with the lowest quartile of cumulative exposure. The associations between quartile of cumulative exposure and ASCVD events after age 40 years were robust to adjustment for the first measurement of non–HDL-C or LDL-C during early adult life, suggesting that when measuring atherogenic lipids in young adults, there may be added prognostic value to knowing the cumulative exposure during early adult life. Interestingly, the values of non–HDL-C and LDL-C that have the highest sensitivity to predict being in the top quartile of cumulative lipid exposure are substantially lower than levels one might infer from young adult single measure age-specific percentiles."
"The association between cumulative exposure and incident ASCVD risk is linear, with lower values having lower ASCVD risks. This has 2 important implications. First, it is difficult to identify a specific threshold for non–HDL-C or LDL-C based on future risk alone, because no clear “threshold” value exists below which no risk is observed. Second, despite non–HDL-C values <107 mg/dL and LDL-C values <97 mg/dL predicting being in the lowest non–HDL-C and LDL-C quartiles (respectively), clinical recommendations to patients should still be that “lower is better.” Thus, patients should continue to follow lifestyle habits to keep their cumulative exposure as low as possible during early adult life. Nonetheless, absolute values derived from this analysis may help clinicians and patients better understand the meaning of each individual’s lipid values on an absolute scale. Importantly, the non–HDL-C and LDL-C values that predict high cumulative exposure should not be misinterpreted as threshold values to initiate lipid-lowering therapy, nor should they be considered as targets for therapy. Rather, such thresholds for initiation of lipid-lowering pharmacotherapy and targets for therapy should be derived from interventional studies."

Figure: "Density plot of the first non–high-density lipoprotein cholesterol (non–HDL-C) (A) or low-density lipoprotein cholesterol (LDL-C) (B) measurement made between ages 18 and 30 years in the CARDIA (Coronary Artery Risk Development in Young Adults Study) cohort and the quartile of cumulative exposure from age 18 through 40 years. The blue curve represents the lowest quartile, red and gray are sequentially higher quartiles, and purple is the highest quartile of cumulative exposure. Of note, overlap in the values of the first measurements are present for all 4 quartiles. Thus, substantial reclassification between quartile of first measurement and cumulative exposure in early adult life occurs. However, there is modest overlap between the top and bottom quartiles, demonstrating that a modest percentage of individuals who were in the middle of the distribution at their initial measurement had increases or decreases in lipid levels that put them in the highest or lowest quartile of cumulative exposure by age 40 years"
 Figure: "ROC curves for the prediction of membership in the top or bottom quartile of cumulative exposure to (A) non–HDL-C and (B) LDL-C from age 18 to 40 years by a 1-time measurement made between ages 18 and 30 years. Overall discriminatory capacity is high (c-statistics of 0.93 for all models). The addition of demographic variables, body mass index (BMI), and systolic blood pressure (SBP) yielded very modest effects on the C-statistics. ROC = receiver-operating characteristic".
Figure: "ROC curves for the prediction of membership in the top or bottom quartile of cumulative exposure to (A) non–HDL-C and (B) LDL-C from age 18 to 40 years by a 1-time measurement made between ages 18 and 30 years. Overall discriminatory capacity is high (c-statistics of 0.93 for all models). The addition of demographic variables, body mass index (BMI), and systolic blood pressure (SBP) yielded very modest effects on the C-statistics. ROC = receiver-operating characteristic".
Concluding:
"One-time measures of non–HDL-C and LDL-C obtained between ages 18 and 30 years are highly predictive of cumulative atherogenic lipid exposure through age 40 years. The absolute values of non–HDL-C and LDL-C that best predict a high exposure to atherogenic lipids in early adult life are substantially lower than those derived from studies of middle-aged adults. Our findings may help guide the clinical assessment of lipid-associated risk in adults <40 years of age."
Study:
https://www.jacc.org/doi/10.1016/j.jacc.2024.05.070
LMHR And New Calcium And CT Angiogram Study
What about the new study looking at calcium scores and coronary CT angiograms of lean mass hyper responders? Doesn’t that look promising?
Unfortunately, there are a few major design flaws and problems with this study.
The study wasn’t designed to show any results. They excluded all patients with coronary artery disease. This makes it nearly impossible to show that ASCVD will develop on a short time horizon. You will have to follow these patients for decades to see if any appreciable, and statistically significant ASCVD, ever develops.
Imagine designing a study to see if diabetes will progress but you excluded all diabetics? Or imagine you designed a study to see if dementia would worsen but you exclude all people with dementia. This is obviously very problematic. Especially considering the short length of the study.
The other problem with this study is that they used calcium scoring and CT coronary angiography. Neither of those will show early-stage subclinical atherosclerosis. You cannot see soft plaque that is not encroaching on the lumen of the artery with either of these modalities. Both modalities can only detect advanced atherosclerosis, or very late stage or end stage atherosclerosis.
The way the study is currently designed, you would have to follow these people for 30 to 50 years to see any progress and then compare them to a group that has normal LDL cholesterol. This is neither feasible nor cheap. It will also be difficult to make sure they adhere to this diet.
A better design would have been to take people with an already positive calcium score, and just check it after a few years to see if it increases. This is a very inexpensive and easy way to show progression. It’s also safer for the participants.
As discussed earlier, these studies have already been done and we know the results. Young people with elevated LDL cholesterol, regardless of BMI, insulin resistance, calcium scores, or other factors will all develop atherosclerosis at an accelerated rate.
Young And Full Of Disease
In July of 2024 an article was published in the Journal of the American College of Cardiology that wanted to answer this exact question. Can young people without any of the traditional risk factors still get heart disease? And what causes it?
They looked at adults aged 40 to 65 that had a 10 year risk score of less than 5%, meaning their risk for ASCVD is very low when looking at the traditional risk factors, age, weight, BMI, diabetes, smoking, kidney function, metabolic parameters, and other metrics. By all objective measures, these were people with a very low risk of heart disease.
They even looked at the presence of calcium or soft plaque in the heart.
They found that most had plaque and it was worse and more prevalent the higher the LDL-C or apoB. The graphics from this paper are quite impressive and I highly recommend you take a look in the supplemental guide.
They also found that for every 10 mg/dL increase in LDL-C or apoB, you had a 13% and 20% increase in ASCVD, respectively. As an example, nearly 70% of men with an apoB over 120 mg/dL had ASCVD. The number was 60% for LDL-C over 160 mg/dL.

They concluded,
“Among healthy asymptomatic middle-aged adults without traditional ASCVD risk factors in the U.S., coronary atherosclerosis on CCTA is common even at lower serum levels of LDL-C, non-HDL-C, and apoB. Coronary atherosclerosis is more prevalent at higher levels of serum lipoproteins for both men and women, and high-risk plaque features are present but relatively infrequent in low-risk adults. These findings emphasize the importance of lipid-lowering strategies to prevent the development and progression of atherosclerosis in adults regardless of risk factors”.
Study:
https://www.jacc.org/doi/10.1016/j.jacadv.2024.101049
Did You Like This Article?
This post is a chapter from my new Cholesterol Book. If you want updates on when that book will be ready for purchase, click on my updates link and sign up to receive updates:
Power of 3 Bundle
Grab My 5 Step Quick Guide for Weight Loss & My Ultimate Macro Counting Guide & My Ultimate Lipid Guide for FREE! Normally a $197 Bundle!
Everything you need to live a healthy life, live longer, and lose weight properly!
Most of my clients, friends, and patients lost all the weight they ever wanted with this bundle!
I hate SPAM. I will never sell your information, for any reason.